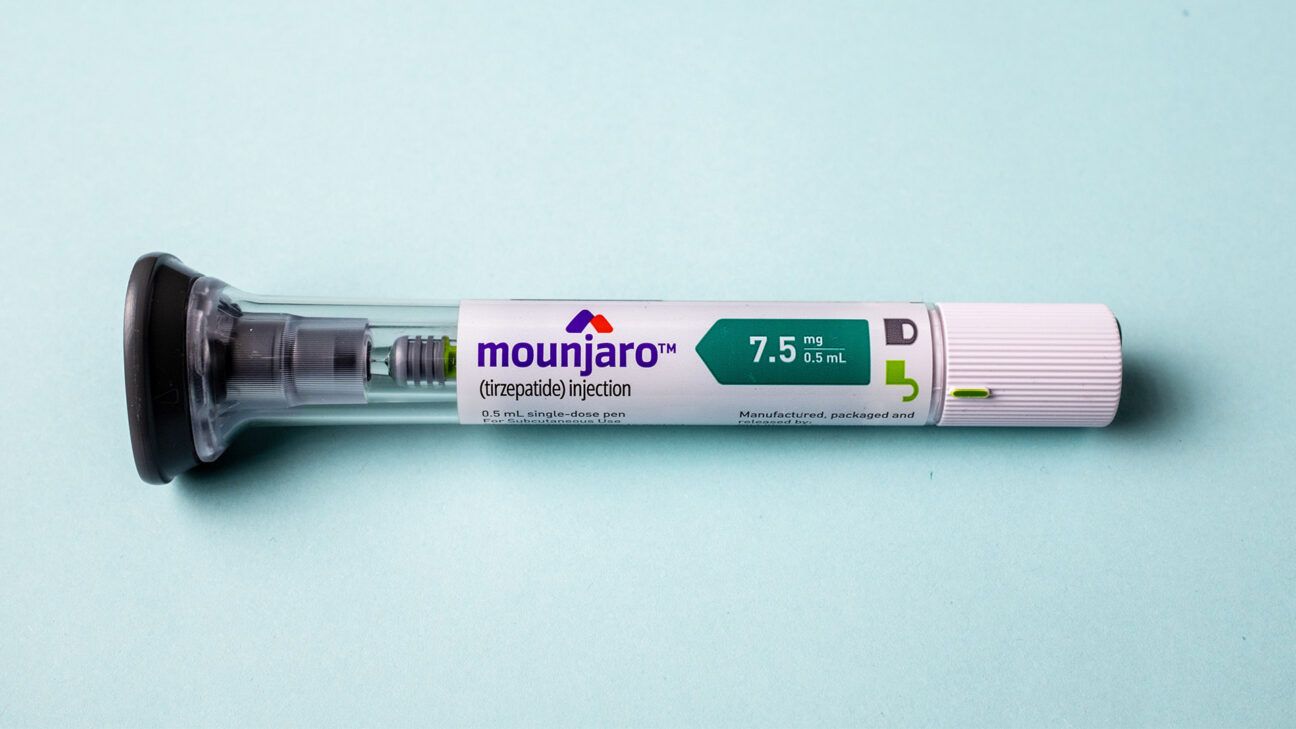
- Tirzepatide, Mounjaro, is already a primary type 2 diabetes medication, but could also work as an adjunct treatment, according to new research.
- The drug appears even more safe and effective than fast-acting insulin in the treatment of uncontrolled type 2 diabetes.
- The findings come from a new clinical trial sponsored by Eli Lilly, the maker of Mounjaro.
For individuals whose type 2 diabetes is hard to control, physicians may be able to turn to a new treatment.
Tirzepatide, commonly known by the brand name Mounjaro, is currently prescribed as a primary treatment for diabetes.
However, a new clinical trial indicates that the medication could also work as an adjunct therapy for individuals who are prescribed both slow-acting insulin and fast-acting insulin at meal times. Results from the trial indicate that tirzepatide, when added to a regimen of slow-acting insulin, was more effective than fast-acting insulin in lowering A1C, aiding in weight loss, and had less incidences of hypoglycemia in people with uncontrolled diabetes.
Researchers published those conclusions today in the medical journal JAMA based on their findings in the SURPASS-6 randomized clinical trial. The clinical trial was sponsored by Eli Lilly, the pharmaceutical company that developed Mounjaro.
“Tirzepatide as an add-on to basal insulin treatment at individual and pooled doses resulted in statistically significant and clinically significant reductions in mean HbA1C…This glycemic efficacy was associated with weight loss and a lower rate of clinically significant hypoglycemia,” the authors wrote.
The results of the trial were praised by the American Diabetes Association:
“The ADA Standards of Care recommends personalized weight loss goals for those with diabetes and obesity. Previous research has shown Tirzepatide to be an effective medication option for lowering body weight in a clinically meaningful way. The results of SURPASS-6 further support the role of Tirzepatide in treatment of individuals with type 2 on insulin and obesity.” Dr. Robert Gabbay, Chief Science and Medical Officer at the American Diabetes Association, told Healthline.
An alternative to fast-acting insulin?
The primary goal of the trial was to determine if tirzepatide was as safe and effective as fast-acting insulin in lowering A1C over 52 weeks. Weight loss or prevention of weight gain was a secondary outcome observed in the trial.
The “open label” trial included 1,428 participants and was conducted between October 2020 and November 2022. Open label refers to the fact that both participants and doctors were aware of the drug being administered. Patients had to be at least 18 years old and have an A1C level of between 7.5% and 11%.
In diabetes care, A1C is shorthand for hemoglobin A1C or HbA1c, which is the amount of hemoglobin in your blood that has sugar (glucose) bound to it over the past three months.
The higher the percentage, the higher your blood glucose levels. A normal A1C range is below 5.7%; prediabetes is 5.7-6.4% and diabetes is defined by an A1C level of anything 6.5% or above, according to the National Institute of Health.
All participants in the trial were prescribed a baseline slow-acting insulin (insulin glargine). Some were then “randomized” to receive either additional fast-acting insulin (insulin lispro) or one of three different doses of tirzepatide (5mg, 10 mg, or 15mg). Once randomized to different intervention groups, the participants were observed for 52 weeks.
At the end of that period, researchers observed how the different tirzepatide doses compared with the fast-acting insulin, individually and as a pooled cohort. They found that the pooled group (all the participants that received tirzepatide), had a mean change of -2.1% compared with -1.1% in those who took fast-acting insulin — almost double. The percentage change in lowering A1C was also dose dependent. Those who took 5mg of tirzepatide saw a -1.9% change in A1C compared with -2.2% for those taking 10mg, and -2.3% in the 15mg group.
The researchers also wanted to see how many participants could reach a specific A1C threshold of 6.5%, which would signal a shift into the prediabetic range for blood glucose. More than half (56%) of those treated in the pooled tirzepatide group reached this threshold, while only 22% in the fast-acting insulin group did. An additional threshold of 5.7%, which would put participants in a normal, healthy A1C range, was also explored: 18% of those in the tirzepatide group reach this threshold while only 3% in the fast-acting insulin group reached a healthy range.
Dr. Marina Basina, Clinical Professor of Medicine- Endocrinology, Gerontology, and Metabolism at Stanford Medicine, said the study showed how the drug can be an alternative help to people when short-acting insulin isn’t controlling blood sugar levels. Basina was not involved in the study.
“Fasting glucose levels were also more significantly decreased in Moujaro treatment groups comparing to mealtime insulin. Interestingly, basal insulin dose was reduced by 30% at the time of the initiation of the medication comparing to our usual clinical practice to reduce the dose by 10-20%,” Basina said. “This fact is encouraging that we can be more aggressive with lowering insulin dose when we initiate the medication.
Significant weight loss
Weight loss was also a significant outcome from the trial, though perhaps that shouldn’t have been a surprise.
Tirzepatide belongs to a class of drugs known as glucagon-like peptide-1 receptor agonists, or GLP-1s for short, the same class of drugs as Ozempic and Wegovy, two blockbuster drugs touted for the treatment of obesity. The key ingredient in those drugs is semaglutide not tirzepatide, but both are GLP-1s and share similarities in how they interact with the body.
A prior study found that Mounjaro was even more effective for weight loss than Ozempic.
After 52 weeks, participants in the pooled tirzepatide group lost about 20 pounds. Meanwhile, those taking fast-acting insulin gained about five pounds. Like other outcomes, weight loss was also dose-dependent, with participants taking higher doses of tirzepatide losing more weight: 22 pounds for those taking 15mg and about 13 pounds for those taking 5mg.
Fewer instances of serious low blood sugar
Safety was also a core focus of the trial, specifically instances of hypoglycemia (low blood sugar), a potentially life-threatening outcome from diabetes medication.
Eighteen deaths occurred during the trial, although none were considered to be related to the study itself.
While there were overall more adverse events among those that took tirzepatide, there were more serious adverse events among those that took fast-acting insulin, of which hypoglycemia was the most common.
Tirzepatide showed significantly fewer instances of clinically significant hypoglycemia or low blood sugar than the fast-acting insulin group. Hypoglycemia was reported in 12% (5mg), 9% (10mg), and 11% (15mg) of participants taking tirzepatide.
Meanwhile, nearly half (48%) of participants in the fast-acting insulin group experienced hypoglycemia.
Similar to other GLP-1s, gastrointestinal issues were the most common reported side effects of tirzepatide; reports most frequently included mild to moderate severity nausea, vomiting, and diarrhea.
The bottom line
Tirzepatide known by the brand-name Mounjaro, appears to be a safe and effective adjunct therapy to slow-release insulin in the treatment of uncontrolled diabetes.
The findings are based on the SURPASS-6 randomized clinical trial sponosred by Eli Lilly, the makers of Mounjaro.
Participants in the trial who used tirzepatide had better improved A1C, lost more weight, and had less instances of hypoglycemia than those who used fast-acting insulin.
Mounjaro May Be Better than Fast-Acting Insulin for Uncontrolled Type 2 Diabetes
Source: Pinoy Lang Sakalam



0 (mga) komento:
Mag-post ng isang Komento